a Department of Psychiatry, University of Rochester School of Medicine and Dentistry, 300 Crittenden Blvd., Rochester, NY, 14642, USA
b Departments of Psychiatry and Pediatrics, Univeristy of Rochester School of Medicine and Denistry, Rochester, NY, USA
c Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
d Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL, USA
e Department of Medicine, The University of Chicago Biological Sciences, IL, USA
f Department of Public Health Sciences, The University of Chicago Biological Sciences, IL, USA
g U.S. Air Force, Head Quarters Air Force, Office of Integrated Resilience, The Pentagon, Washington, DC, USA
h U.S. Air Force Surgeon General’s Office, Now with Syracuse Veterans Affairs Medical Center, Syracuse, NY, USA
U.S. military suicides are increasing and disrupted relationships frequently precede them. Group-level interventions are needed that reduce future suicide vulnerability among healthy members and also ameliorate risk among those already suicidal. We examined whether our Wingman-Connect Program (W-CP) strengthened Air Force relationship networks and socially integrated at-risk members. Air Force personnel classes in training were randomized to W-CP or active control (cluster RCT), followed up at 1 and 6 months (94% and 84% retention). Data were collected in 2017–2019 and analyzed in 2020–2021. Participants were 1485 male and female Airmen in 215 technical training classes. W-CP training involved strengthening group bonds, skills for managing career and personal stressors, and diffusion of healthy norms. Active control was stress management training. Primary outcomes were social network metrics based on Airmen nominations of valued classmates after 1 month. Baseline CAT-SS >34 defined elevated suicide risk. W-CP increased social network integration, with largest impact for Airmen already at elevated suicide risk (n = 114, 7.7%). For elevated risk Airmen, W-CP improved all network integration metrics, including 53% average gain in valued connection nominations received from other Airmen (RR = 1.53, 95% CI = 1.12, 2.08) and eliminated isolation. No elevated risk Airmen in W-CP were isolates with no valued connections after 1-month vs. 10% among controls (P < .035). In contrast to at-risk controls, at-risk WCP Airmen increased connections after intervention. W-CP’s effect on a key indicator, ≥2 connections, was still greater 2–4 months after classes disbanded (6-months). Wingman-Connect Program built enhanced suicide protection into unit relationship networks and counteracted standard drift towards disconnection for at-risk Airmen, despite no explicit content targeting connections specifically to at-risk Airmen. Findings support a growing case for the unique contribution of group-level interventions to improve social health of broader military populations while also ameliorating risk among individuals already at elevated suicide risk.
* Corresponding author. Department of Psychiatry, University of Rochester School of Medicine and Dentistry, 300 Crittenden Blvd., Rochester, NY, 14642, USA.
E-mail address: peter_wyman@urmc.rochester.edu (P.A. Wyman).
1 This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. W81XWH-14-1-0322. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
2 Time supported by K23MH101449.
https://doi.org/10.1016/j.socscimed.2022.114737
Received 29 October 2021; Received in revised form 15 December 2021; Accepted 19 January 2022
Available online 22 January 2022
0277-9536/© 2022 University of Rochester School of Medicine and Dentistry. Published by Elsevier Ltd. This is an open access article under the CC BY-NC-ND
license (https://creativecommons.org/licenses/by-nc-nd/4.0/).
U.S. military suicides increased 50% from 2008 to 2018 (16.1–24.8 per 100,000) (Pruitt et al., 2019). After decades of lower suicide rates in this group, U.S. military suicide rates are now equal to the general population (Hoge, 2019). Existing military prevention efforts focus primarily on identifying and treating those who are already suicidal or at high risk (Comtois et al., 2019; Rudd et al., 2015). Although this approach is clearly necessary and has undoubtedly saved lives, it is also insufficient on its own (Rose, 1985; Brown et al., 2007; Wyman, 2014). To significantly reduce suicide rates, broader group-level interventions are required to (a) reduce vulnerability for future suicidal behavior in large collections of healthy service members, and (b) ameliorate risk among those already with suicidal thoughts and behaviors, most of whom do not seek treatment (Hom et al., 2017; Martin et al., 2019).
The Wingman-Connect Program (W-CP) is the first universal preventive intervention tested through a randomized clinical trial to reduce suicide risk and depression in a general, non-clinical U.S. Air Force population (Wyman et al., 2020) Consistent with the imperative to address needs of both healthy and vulnerable service members alike, W-CP targets the relationship networks that military personnel are embedded within, through a network health approach (Wyman et al., 2019). The W-CP’s group training focuses on two suicide-protective functions of networks. First, strengthening connections among group
members, especially those isolated from the network, to augment protective effects of healthy bonds (Rugo et al., 2020; Silva et al., 2016). Second, building each group’s collective skills for managing career and personal challenges, to create a healthy group culture that leverages the influence of peers on members’ behaviors including their help seeking and coping (Wyman et al., 2019; Pickering et al., 2018; Valente, 2010). A cluster RCT with Air Force personnel in training showed W-CP increased Airmen’s perceptions of belonging to more cohesive, healthy groups, which helped reduce suicide risk and depression (i.e., mediated intervention impact) (Wyman et al., 2020)
This framework is motivated by substantial empirical and theoretical evidence that underlines the importance of individuals’ surrounding social networks for suicide risk and mental health (Tsai et al., 2015; Wyman et al., 2019; Mueller et al., 2021). Military service poses specific challenges to the health of relationships (e.g., frequent relocations) (Burrell et al., 2006; IOM, 2013), and peers are frequently the sole source of help seeking and help receiving in a situation where formal treatment services are significantly underutilized (Hom et al., 2017; Martin et al., 2019). Relationship disruptions, for example, are the most common psychosocial stressor preceding military suicides (Pruitt et al., 2018). Compounding these challenges, findings presented below also show that in the absence of intervention, the expected course for suicidal Airmen is towards increasing social isolation. Conversely, service members embedded within more cohesive units report less suicidal ideation both concurrently (Griffith, 2015; Rugo et al., 2020) and prospectively (Anderson et al., 2019) and reduced vulnerability following combat exposure (Campbell-Sills et al., 2020). This evidence also clarifies several suicide-protective mechanisms of cohesive, connected networks (Wyman et al., 2019; Mueller et al., 2021), including direct effects of social bonds on psychological health (Whitlock et al., 2014) and group norms that incentivize adaptive behaviors and coping (e.g., responsible substance use) (Mead et al., 2014).
The present study thus tested whether Wingman-Connect Program achieved the objective of strengthening the network structure of unit relationships over time, including socially integrating those currently at elevated risk for suicide. This is an especially important hypothesis since W-CP training has no content encouraging Airmen to form connections with at-risk peers. Specifically, we utilized social network analysis techniques (e.g. (Valente, 2010; Wasserman and Faust, 1994)) to evaluate whether Wingman-Connect Program improved established metrics of network integration among both healthy Airmen and Airmen who were at elevated suicide risk at the onset of the intervention (i.e., baseline). We used metrics that emphasized Airmen’s direct first-degree connections with one another (i.e., total ties, density of ties), as those are posited to have the most impact on the health of each individual Airmen, and due to the relative lack of higher degree, distal connections in the small technical training classes (n = 8–15 members). We predicted both lower risk and elevated risk groups would improve on these network metrics (relative to an active control condition), with the greatest improvement among Airmen at elevated suicide risk prior to intervention exposure at baseline.
This study used social network data collected within a cluster RCT testing efficacy of the Wingman-Connect Program with Air Force personnel at the Technical Training School, Sheppard Air Force Base, Wichita Falls, Texas (trial protocol in Supplement 1). Recruitment and baseline assessments occurred between Oct 2017–Mar 2019. One-month follow-up was in the final weeks of technical training; 6-month follow up occurred two to four months after classes disbanded and each Airmen had transferred to their first operational base assignment. Study procedures were approved by the U.S. Department of Defense and University of Rochester IRBs. All participants provided written informed consent and were compensated $50. The trial was registered at ClinicalTrials.gov (NCT04067401).
A CONSORT diagram (Fig. 1) shows the flow of randomized classes and the social networks of Airmen embedded within them. Airmen is the generic Air Force term used to describe all personnel. Those social networks include Airmen enrolled as research subjects – as well as all remaining class members who did not provide data but received nominations as part of the class social network. Note, from this same RCT we previously presented a CONSORT diagram showing flow of individual research participants, as part of analysis of intervention impact on individual-level outcomes including suicide risk.(Wyman et al., 2020) Class units from the same squadron were matched (job classification, size, duration) and one class from each pair was randomly assigned to W-CP and the other to a stress management training. Intervention group assignments were unknown to participants or research personnel until after enrollment and baseline assessments. An active comparison training was used to strengthen internal validity including controlling for contact with external trainers.
Eligible participants were all Airmen in 216 technical training classes (Mean size: 6.9; range: 4–13) in two squadrons: 365 Avionics and 363 Weapons Systems. These are full-time intensive courses to prepare personnel for their Air Force jobs. Of 1897 eligible Airmen in 216 classes, 1485 enrolled from 215 classes: 748 in classes assigned to Wingman-Connect and 737 in classes assigned to stress management. The enrolled sample (1222 male; 253 female; Mean age 20.9 years) was representative of the training school population. Follow-up retention rates were 94% at 1-month and 84% at 6-month, and did not vary by training condition.
A total of 398 remaining Airmen were randomly assigned to an intervention condition as part of their classes but did not enroll as subjects or complete data collection steps (180 W-CP, 218 stress management). Note, these non-enrolled members are part of the network intervention mechanism and they are incorporated in the social networks constructed for each class.
Each Airmen at the time of enrollment was given information covering Air Force mental health and family support resources as well as a crisis call-line. That information was repeated through the online survey. Airmen were informed that individual CAT-SS responses would not examined for the purpose of crisis response and those responses would be de-identified at the earliest opportunity prior to being sent to the study team.
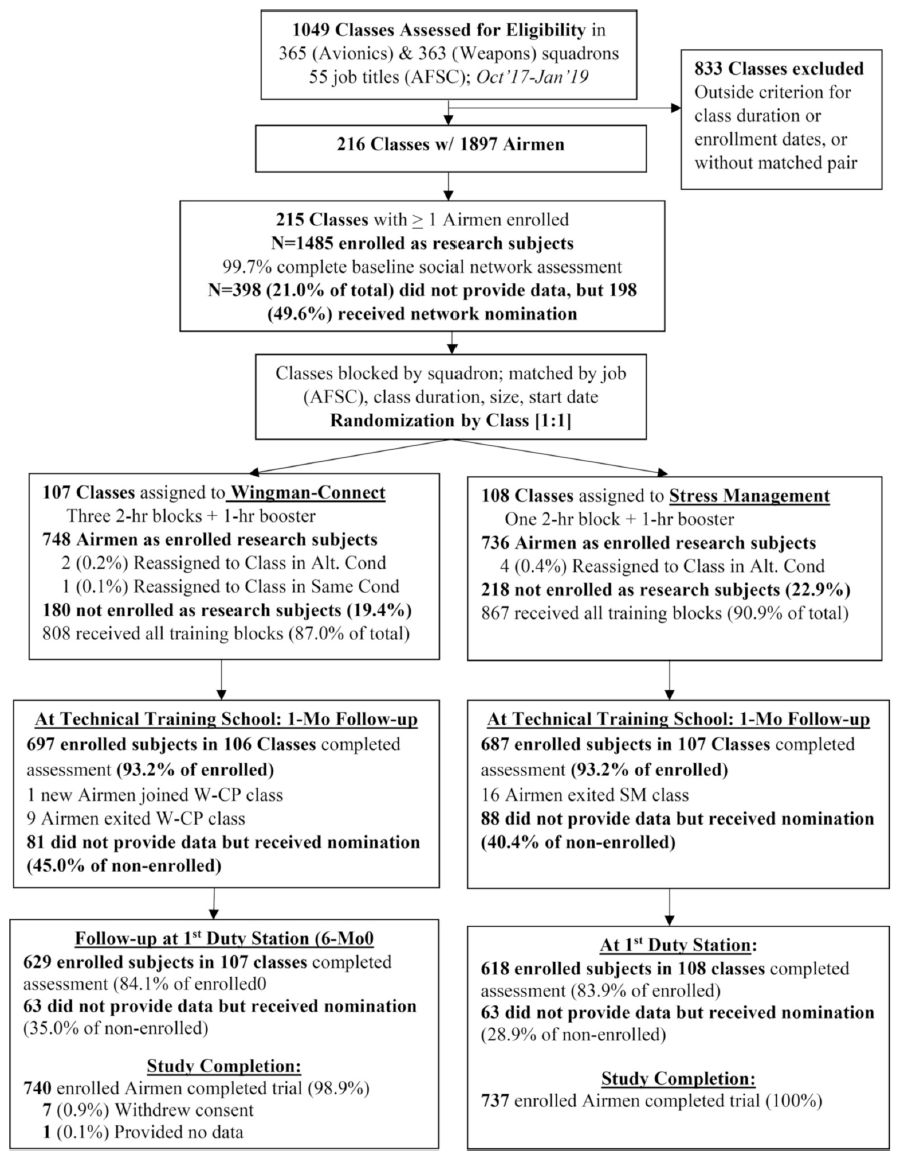
Fig. 1. Flow of randomized technical training classes and the social networks of Airmen embedded within them in the Wingman-Connect Trial.
The Wingman-Connect Program trains all members of natural organizational units together to strengthen group bonds and the diffusion of suicide-protective norms and practices (three 2-hr training blocks). Skill-building activities focus on relationships and practices supportive of mental health, theoretically linked to reduced suicide risk, and essential to an Airman’s job success (Wyman et al., 2020). Specific modules and activities build healthy relationships and accountability (Kinship), meaning and value in work and life (Purpose), informal and formal help-seeking (Guidance), and activities that give strength (Balance). Group skill-building activities identify strengths of all group members, and members learn how a strong network supports all members’ health and fitness. W-CP uses high energy activities and peer-to-peer teaching; exercises inside and outside of training promote adoption of skills into unit culture.
Stress management training consisted of an overview of the stress response system, the impact of stress on health, and cognitive and behavioral stress management strategies drawn from a cognitive behavioral therapy workbook (Leahy, 2018). The trainer used a slideshow to introduce the information, show videos and lead groups in practice of a guided relaxation and interactive discussion (2 h total). Stress management was selected in consultation with USAF partners as the active control training based on similarity in delivery style and content to other U.S. military prevention trainings.
Participants in both conditions received training-specific informational messages for 6 months. Trainers of both interventions had varied backgrounds (education, mental health) and education levels (bachelor’s and master’s level) from the research team. Data on training fidelity has been reported previously (Wyman et al., 2020)
This study’s primary outcomes were indices of social network integration (see below). Previously reported outcomes for this trial included self-report measures of suicide risk, depression and occupational fitness problems (Wyman et al., 2020) This study used suicide scale (CAT-SS) scores of the Computerized Adaptive Test for Mental Health (Gibbons et al., 2017) collected at baseline to identify Airmen at elevated risk for suicide. The CAT-SS administers a statistically optimal subset of items from a bank of 111 items from validated scales syndromally associated with suicidal thoughts and behaviors. Across the range of CAT-SS scores (0–100) there is a 52-fold increase in likelihood of current suicidal ideation validated against clinician assessment on the Columbia Suicide Rating Scale (C-SSRS). CAT-SS also yields categorical scores (low, medium, and high); a 1-category change corresponds to a 16 times greater likelihood of an increase in C-SSRS’s ordinal scale. We combined medium and high categories for this non-clinical sample. Airmen with a suicide scaled score greater than 34 were considered at elevated risk for suicide.
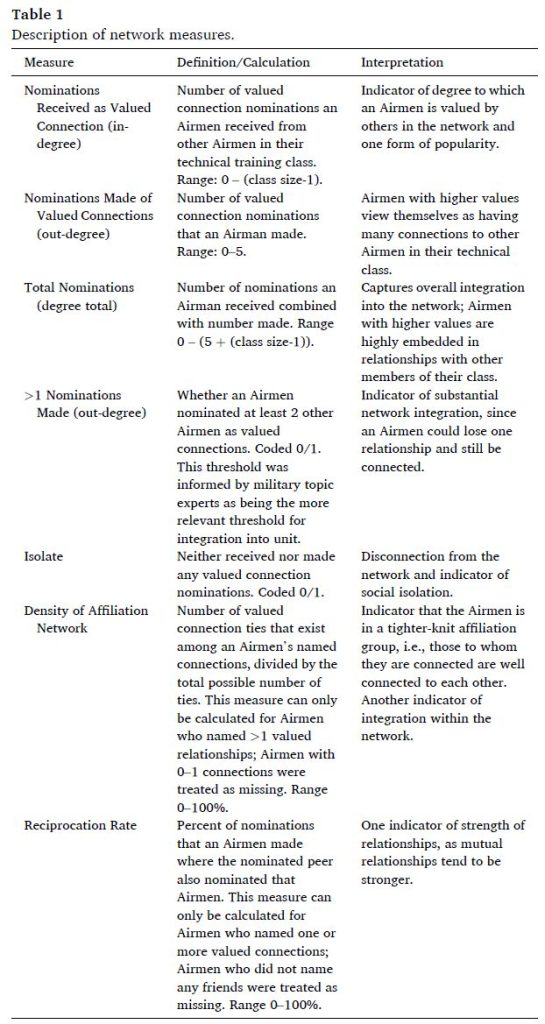
Network Construction. Airmen named up to five members of their technical training class whom they respect and would choose to spend time with: Valued Connections. Wording for nominations was reviewed and approved by topic experts to capture valued connections in the context of USAF training culture. Nominations were made at each assessment point. Writing in nominations yields fewer, yet closer relationships versus checking names off a roster (Valente et al., 2009). Airmen could name all class members including Airmen who did not choose to enroll as research participants (21.1% of any class in either condition).
Network Measures. Valued connection nominations from each Airmen (i.e., ego) to other Airmen (i.e., alters) were used to construct social network graphs of each class, on which network metrics were computed. The collection of metrics used in this study is given in Table 1.
Choice of Primary Measure and Longitudinal Timeframe. This study’s primary outcomes were network integration metrics one month after intervention while Airmen were still embedded in technical training school classes. We examined network variables at 6-month follow-up as secondary outcomes to assess retention of valued connections among former classmates.
Choice of Primary Measure and Longitudinal Timeframe. This study’s primary outcomes were network integration metrics one month after intervention while Airmen were still embedded in technical training school classes. We examined network variables at 6-month follow-up as secondary outcomes to assess retention of valued connections among former classmates.
Network measures were created using R statistical software 3.6.3 (R_Core_Team., 2020) with the igraph package (Csardi and Nepusz, 2006). Network diagrams were graphed using the tidygraph package. All other analyses were conducted in R. We tested differences between Airmen with and without elevated suicide risk on baseline network and demographic variables using Wilcoxon rank-sum test, Fisher’s exact test, and chi-square test of independence.
To test the effect of W-CP vs. stress management training, we constructed generalized linear mixed-effects regression models predicting each social network metric at the 1-month follow-up (and, as secondary analysis, the 6-month follow-up) adjusting for baseline values of each respective metric. These intention-to-treat (ITT) models were adjusted for gender and group size (linear and quadratic) and included a random intercept for group to account for the nesting of Airmen within technical training classes, which were the unit of randomization and of intervention. Previous analyses accounting for random class effects showed baseline equivalence of the randomized W-CP and stress management groups. We additionally examined whether the intervention had differing effects on social network metrics for individuals at elevated risk for suicide by adding an intervention-by-risk interaction term. Upon finding significant interactions, we reported the risk-group-specific estimates, where appropriate. The link function for these models was contingent on the distribution of the outcome variable (e.g., “Poisson” for in-degree, “Binomial” for isolate status, “Identity” for density). Residuals and model fit statistics (e.g., Pearson’s goodness of fit) were checked to ensure the model fit well and the appropriate link function was used. For each social network metric, we additionally tested for significant interactions of training condition by baseline network metric to determine if W-CP had differential impact for Airmen entering with higher or lower network metrics.
To determine the typical trajectory for Airmen at elevated suicide risk, we examined a 3-way interaction combining the moderating effect of suicide risk status by intervention condition by time. This involved examining the effect of time on total valued connection nominations (i. e., rate ratio for 1-month vs. baseline) specific to each treatment condition by suicide risk status. The primary interest was the difference in time effect (i.e., ratio of rate ratios) for Airmen at elevated vs. not elevated suicide risk within the control condition, as well as in W-CP condition.
To study the intervention effects on dynamic connections in these networks, we computed separate “addition” and “removal” networks. These consisted of valued connection nominations that were either 1) added from baseline to 1-month follow-up, or 2) removed from baseline to 1-month follow-up. We treated the “addition” and “removal” networks as separate discrete networks and used the modeling approach described above to assess intervention effects on addition or removal metrics.
A total of 114 Airmen in the study population (7.7%) were at elevated suicide risk (CAT-SS scores >34) (see Table 2). Airmen at elevated risk were equivalent on demographic characteristics to those not at risk yet directionally less integrated into their class networks at baseline, i.e., fewer nominations received (1.68 vs. 1.95; P = .057) and higher proportion of isolates (6.1% vs. 2.8%; P = .081). Baseline differences were consistently found on social functioning and mental health prior to the intervention onset. Specifically, Airmen at elevated suicide risk vs. not at risk were significantly more likely to have elevated depression symptoms (93.9% vs. 12.2%), loneliness, emotion regulation difficulties, anger, and scores on military functional impairment-social scale (see Supplemental Table S1).
Wingman-Connect counteracted the typical drift towards disconnection for Airmen at elevated suicide risk. Findings from the control condition indicated that the typical trajectory for Airmen with elevated suicide risk was towards decreasing connections and increasing isolation. Specifically, Airmen in the active control condition who were at elevated risk showed a significant decline in total valued connections of 19% compared to Airmen not at risk (RR = 0.81, 95% CI = 0.66, 0.99; P = .047). In contrast, in Wingman-Connect trained groups there was a non-significant trend such that more valued nominations were maintained among at-risk Airmen compared to non-elevated counterparts (RR = 1.14, 95% CI = 0.92, 1.41; P = .23). Fig. 2 shows average total valued connections at baseline and 1-month for Airmen at elevated suicide risk vs. not at risk for active controls (left) and W-CP (right).
Wingman-Connect increased measures of network integration, with larger and broader impact for Airmen at elevated risk of suicide (see Table 3 for results of primary outcome analyses).
Compared to Airmen in the active control training, W-CP trained Airmen were significantly more likely on average to name at least two classmates as valued connections, the benchmark for unit integration set by military subject matter experts (OR = 1.40; 95% CI = 1.11, 1.78; P < .005), and the density of affiliation group was higher (B = 0.08, 95% CI = 0.05, 0.12; P < .001).
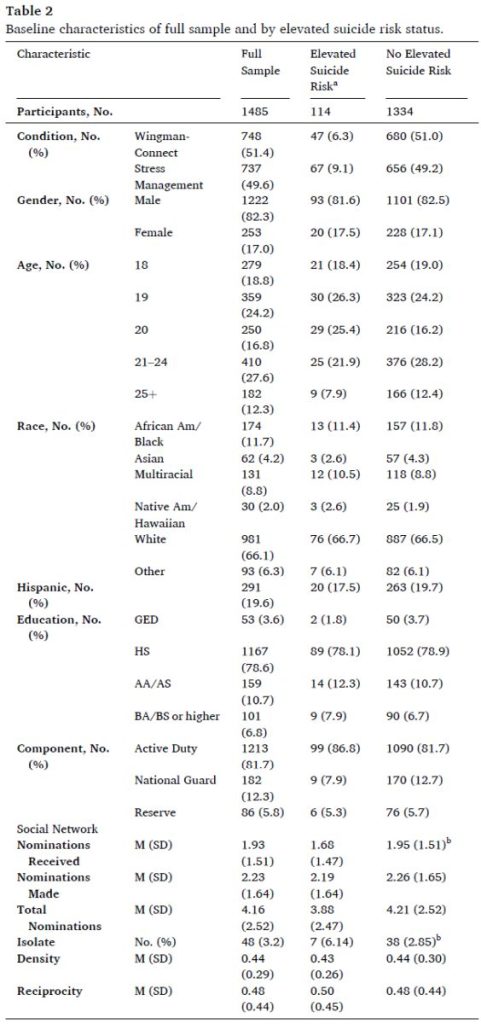
No statistically significant (p < .05) differences between Airmen with and without elevated suicide risk on any demographic or social network variable.
Some percentages do not equal 100% because of missing data.
a At baseline, 37 participants did not complete the CAT-SS and are missing data
on suicide risk.
b Differences in network characteristic by elevated suicide risk status p < .10.
Wingman-Connect increased valued connection nominations received and made the most for Airmen beginning with fewest connections, as shown by significant training condition by baseline interactions. For Airmen with 0 or 1 valued connection nominations received at baseline, nominations received was on average 1.19 times (RR = 1.19, 95% CI = 1.02, 1.39) and 1.13 times (RR = 1.13, 95% CI 1.01, 1.27) as high, respectively, for W-CP vs. stress management. I=n contrast, treatment impact on nominations received was not significant for those with 2 or more nominations at baseline. A similar interaction effect was found for valued connection nominations made: W-CP had positive impact for Airmen starting with 0 (RR = 1.86, 95% CI = 1.22, 2.84), one (RR = 1.65, 95% CI = 1.21, 2.24), or 2 (RR = 1.45, 95% CI = 1.14, 1.85) nominations made, but impact was not significant for those with 3 or more nominations.
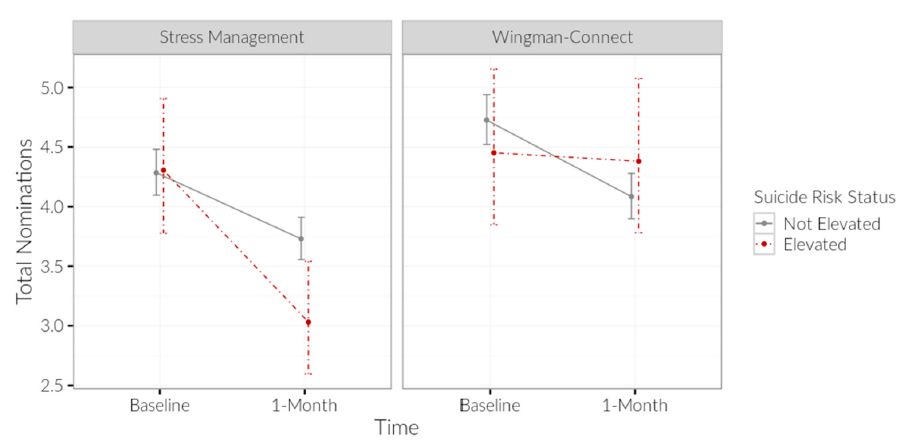
Fig. 2. Total Valued Connection Nominations at Baseline and One Month Follow-up for Airmen at Elevated Suicide Risk Status vs. Not in Active Control (left) and Wingman-Connect (right).
For Airmen at elevated risk of suicide, Wingman-Connect training increased all nomination metrics relative to the active control condition: nominations received from classmates was greater by 53% on average (RR = 1.53, 95% CI = 1.12, 2.08); P = .007), nominations made was greater by two-thirds of a classmate (B = 0.68, 95% CI = 0.13, 1.24; P .02), and total nominations was increased by approximately 40% (RR =1.41, 95% CI = = 1.14, 1.74; P < .001). Airmen at risk in W-CP classes were three times as likely to name at least two valued connection classmates (61% vs. 34%) (OR = 2.94, 95% CI = 1.21, 7.14; P < .02). Wingman-Connect eliminated isolation for at-risk Airmen (i.e., no valued connection nominations made or received to or from classmates). At 1-month follow-up, none of the at-risk Airmen were isolates in W-CP vs. one in 10 Airmen (10%) in the active control condition (P < .035). Due to zero isolates in the W-CP condition and an upper bound of the OR was infinity, confidence intervals for the estimated proportions shown in Table 2 were calculated using Fisher’s Exact Test.
Fig. 3 depicts two illustrative class social networks showing increasing social integration and decreasing isolation for Airmen at elevated suicide risk in Wingman-Connect trained groups (top). In contrast, social integration decreased in active controls, and an Airmen at elevated suicide risk became isolated (bottom).
Results showed that friendship networks were more dynamic – in both additions and removals – in the Wingman-Connect condition (see Fig. 4). Nominations received in the addition and removal networks refers to the number of classmates who added or removed an Airmen, respectively, from their valued connection network between baseline and follow-up. Airmen in W-CP trained groups were on average added by others as new valued connections at 1.16 (95% CI = 1.00, 1.34, P = .047) times the rate compared to controls (adjusted M = 0.50 vs. 0.43 respectively). Likewise, Airmen in W-CP groups were on average removed by others as valued connections at 1.16 (95% CI = 1.03, 1.30, P = .013) times the rate compared to controls (adjusted M = 0.85 vs. 0.74, respectively).
For valued connection nominations made, a strong effect was observed for Airmen with suicide risk: specifically, Airmen at elevated risk in W-CP groups made new valued connection nominations at 2.49 (95% CI = 1.24, 5.00, P = .01) times the rate of at-risk Airmen in the active control condition.
Six-month follow-up occurred 4–5 months after technical training classes graduated and after Airmen had transferred – as individuals not as class units – to operational bases. All W-CP effects at 6-months were in the same direction as 1-month; however, some effects were no longer significant (see Table 4). Overall, the number of valued connections were, as expected, lower 5 months after classes disbanded – roughly half of 1-month.
Six month findings again showed that W-CP offset the typical trajectory of decreasing connections for Airmen at elevated suicide risk. Even months after classes were disbanded, W-CP trained were 33% more likely on average vs. controls to name 2 or more former classmates as valued connections (OR = 1.33; 95% CI = 1.01, 1.75; P < .04), the benchmark for social integration set by military topic experts. This effect is comparable to that at the 1-month while classes were still intact (OR = 1.40). Among controls, 30% fewer Airmen at elevated suicide risk on average named 2 or more valued connections at 6-months vs. those not at risk (OR = 0.70; 95% CI = 0.41, 1.20; P = .19); in contrast, in W-CP trained only 4% fewer at-risk Airmen named 2 or more classmates as valued connections vs. those not at risk (OR = 0.96; 95% CI = 0.58, 1.58; P = .86). Although this finding of decreasing connection among at-risk controls was directionally consistent with the 1-month findings, the result crossed the traditional significance threshold.
To assess the robustness of the findings, we performed a sensitivity analysis described by Frank et al. (2013), using the “konfound” package in R. Results of our sensitivity analysis showed that for this study’s primary effect of the intervention on total nominations for at-risk airmen (b = 1.41, se = 0.14, n = 1485), our Robustness of an Inference to Replacement (RIR) is 80.83%. That is, in order for our previous inference to be totally invalidated, roughly 80% of that effect would need to have been from bias. Given how implausible that would be in this case, we conclude our treatment effect is robust and the most plausible account of the data.
The Wingman-Connect Program (W-CP) improved multiple metrics of social network health for all Airmen, with the greatest benefit for those with elevated suicide risk. For at-risk Airmen, W-CP increased valued connection nominations received from classmates by 53% and eliminated isolation while class units were together in training. These findings are especially notable given that W-CP had no explicit content targeting at-risk Airmen or encouraging Airmen to form connections with at-risk peers. The findings are also notable given the broad deficits – that would likely impact social network formation and evolution – observed in at-risk Airmen at baseline (e.g., higher anger, depression, emotion regulation difficulties). Nevertheless, for at-risk Airmen in WCP classes other airmen were motivated to form close ties with them and increase their integration into their class networks. Moreover, months after classes were disbanded, W-CP’s effect on a key indicator of network integration (i.e., two or more connections with classmates) was still significantly greater than controls. These effects were achieved through 6 h of group training, with periodic reinforcing text messages. These findings are, to our knowledge, the first to show that a suicide prevention program for small personnel units improved significantly the group relationship network and socially integrated members at elevated risk for suicide over time.
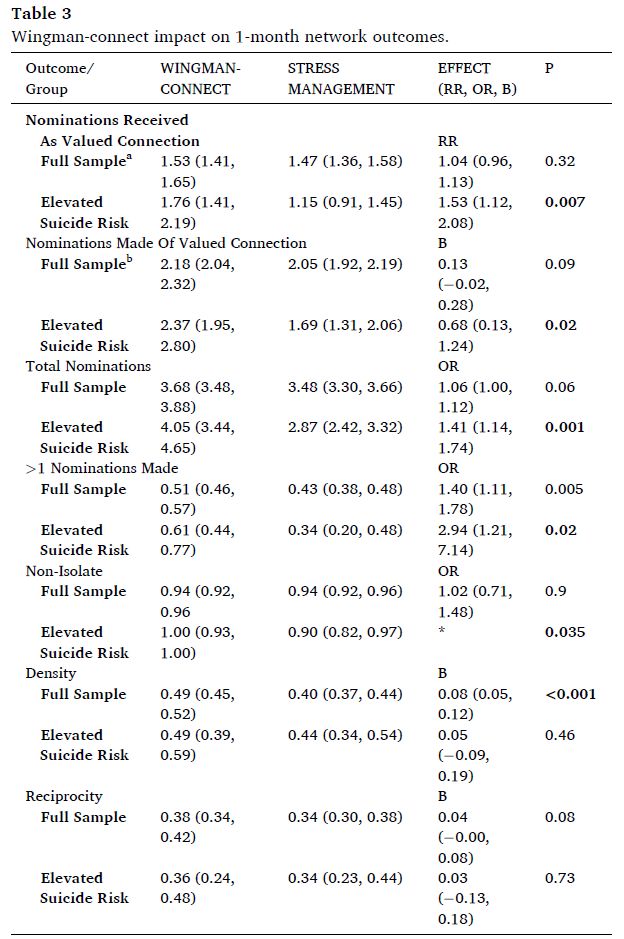
Values show estimated means (nomination metrics), probabilities (dichotomous variables), or percentage (density, reciprocity) at 1-month follow-up, with 95% CIs. Models adjusted for baseline value of each network variable, class (random effect), gender and group size. RR refers to relative rate ratio, OR stands for odds ratio, and B stands for difference in means all adjusted for covariates. Boldface indicates statistical significance (P < .05).
* Infinite point estimate of the odds ratio due to 0 isolates for Airmen with elevated suicide risk in W-CP condition. Test statistic based on 2-sided Fisher’s Exact Test; proportions shown are observed at 1-month.
a Wingman-Connect Program had greater benefit for Airmen with fewer connections at baseline as shown by significant intervention condition × baseline interactions. For Airmen with 0 or 1 valued connection nominations received at baseline, nominations received was on average 1.19 times (RR = 1.19, 95% CI 1.02, 1.39) and 1.13 times (RR = = 1.13, 95% CI = 1.01, 1.27) as high, respectively, for Wingman-Connect Program vs. active control.
b A similar interaction effect was found for nominations made. For Airmen with 0, 1, or 2 nominations made at baseline, nominations made was on average 1.86 times (RR = 1.86, 95% CI = 1.22, 2.84), 1.65 times (RR = 1.65, 95% CI = 1.21, 2.24), and 1.45 times (RR = 1.45, 95% CI = 1.14, 1.85) as high, respectively, for Wingman-Connect Program vs. active control.
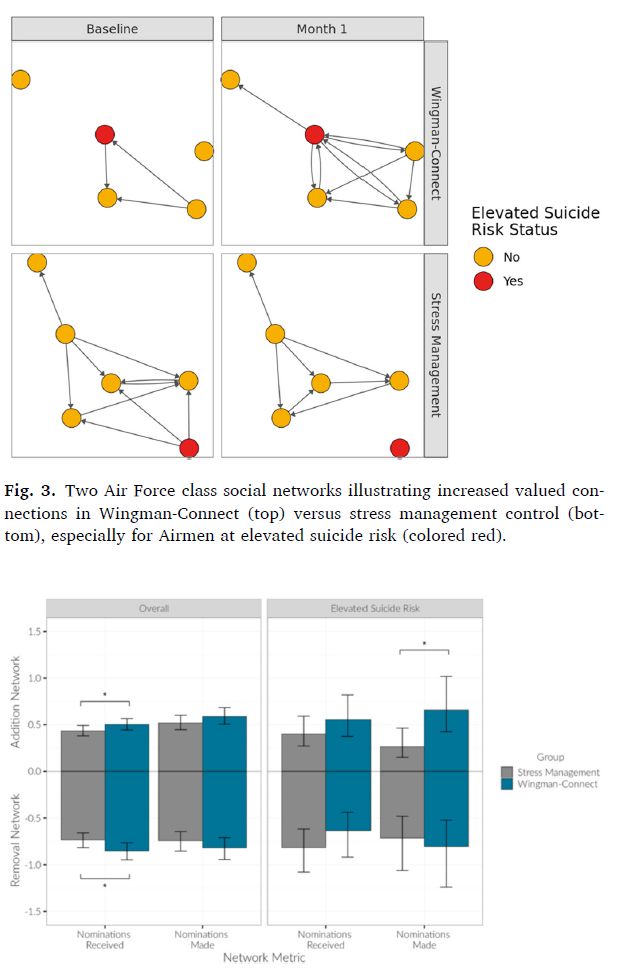
Fig. 4. Addition and Subtraction Networks for Wingman-Connect vs. Control Training by Elevated Suicide Risk Status.
This study extends knowledge of the social and relationship impact of the Wingman-Connect Program as it decreased suicide risk for Airmen in training. Previous findings from this RCT showed W-CP’s effect on reducing suicide risk was mediated by Airmen’s perceptions of being part of more cohesive, healthy units (Wyman et al., 2020) The present analysis anchors the effects on suicide risk to specific improvements in the network of unit relationships. Use of social network methods with 215 technical training classes increases confidence that W-CP effects captured meaningful changes in relationship systems. Social network analysis uses multi-informant indicators of social bonds. Each Airmen’s indicators of network health incorporated independent reports made by other Airmen in their unit. W-CP increased the likelihood that at-risk Airmen would be identified by others as a valued connection.
These findings have implications for the broader suicide prevention paradigm in the United States military. The current attention on the detection and treatment of suicidal military members is necessary, but ultimately insufficient to meet the needs of many suicidal service members. Results from our study suggest that the status quo progression for many service members at elevated suicide risk is one of worsening disconnection, evidenced by the trajectory of declining valued connections found in the active control condition. One in 10 Airmen at elevated suicide risk in the control condition in our study (10%) had no connections to other members at the one month follow-up, approximately two months after technical training classes began. Disconnection from others is a known risk factor for suicide (Silva et al., 2016; Lutz et al., 2021; Van Orden et al., 2010) that the current mental health service paradigm is not designed to address.
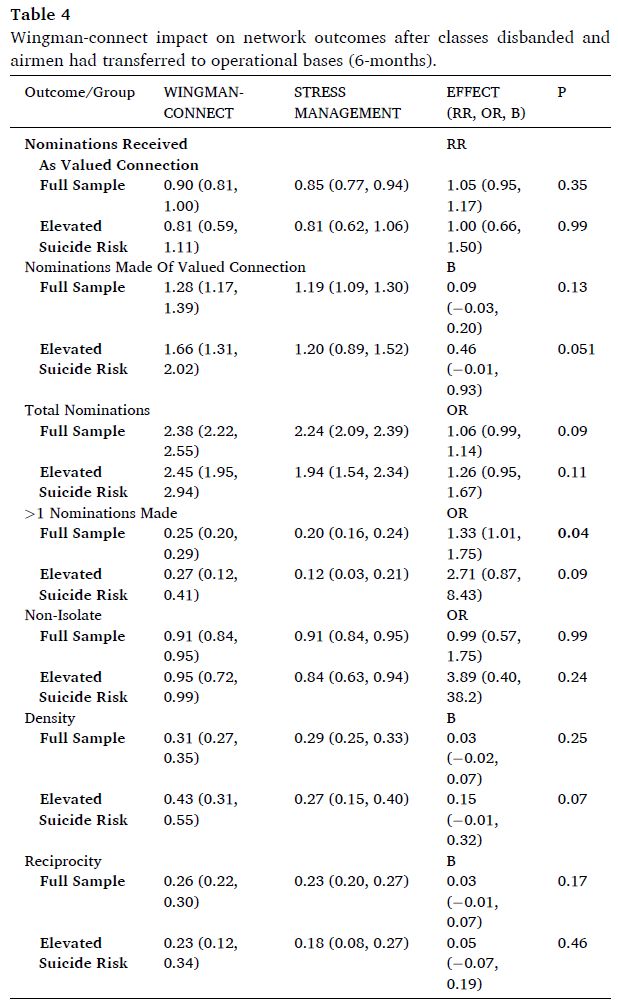
Values show estimated means (nomination metrics), probabilities (dichotomous variables), or percentage (density, reciprocity) at 6-month follow-up, with 95% CIs. Models adjusted for baseline value of each network variable, class (random effect), gender and group size. RR refers to relative rate ratio, OR stands for odds ratio, and B stands for difference in means all adjusted for covariates. Boldface indicates statistical significance (P < .05). *Infinite point estimate of the odds ratio due to 0 isolates for Airmen with elevated suicide risk in W-CP condition. Test statistic based on 2-sided Fisher’s Exact Test; proportions shown are observed at 6-month.
Wingman-Connect Program counteracted the expected drift towards
disconnection for Airmen at elevated suicide risk by targeting the unit’s
relationship network itself. These groups built enhanced suicide protection into their relationship networks, with the most consistent benefits for Airmen at elevated risk of suicide and for those starting with fewest connections. Our findings identify the relationship networks in small military units as a feasible and actionable (i.e., modifiable) target for universal suicide prevention. Suicide protection at the Airmen unit level may also be efficient, with the potential to initiate cascading prevention impacts over time. In more connected, healthier units, vulnerable members can borrow strength from adaptive members. Stronger units also promote job fitness, as shown by W-CP’s impact reducing occupational problems (Wyman et al., 2020), an effect that may reduce future problems that precipitate new instances of suicidal thoughts and behaviors. This finding is especially important in light of previous work showing that depressed individuals may become isolated – at least in part – due to their own social withdrawal (Schaefer et al., 2011). In that sense, W-CP may specifically assist vulnerable Airmen in overcoming barriers to forming meaningful social connections.
This study’s findings suggest a plausible mechanism for W-CP increasing relationship integration: Wingman-Connect Program’s interactive training created more dynamic relationship networks. Airmen in W-CP groups made more changes in who they named as valued connections (i.e., additions and removals of nominations), even as the overall average number of valued connections increased. The largest dynamic changes were for Airmen with elevated suicide risk in W-CP groups, who made on average three times more new valued connection nominations. Prior research has shown the natural process of group formation begins with increased openness to connections, followed by pruning and resulting in crystallized networks (Christakis, 2019). Our findings suggest W-CP may have extended and augmented this dynamic relationship formation process through its interactive training activities.
Study limitations include that Wingman-Connect Program was implemented in technical training classes that are of relatively brief duration. How lasting the network effects are for units already formed and when delivered to units made of more heterogeneous personnel of different ages and experience levels remain to be determined. Neither Airmen nor trainers were blinded to the intervention condition.
This study’s findings support a growing case for the unique contribution of group-level interventions capable of improving the social health of the broader military population while also ameliorating risk among individuals already at elevated suicide risk. Epidemiologic evidence demonstrates that most instances of suicide will come from individuals outside clearly identified high-risk groups (Rose, 1985; Brown et al., 2007), and a majority of military members who die by suicide will not contact the mental health system preceding death (Hom et al., 2017; Martin et al., 2019). Results show the Wingman-Connect Program is a tool with the potential to serve as a core element of a comprehensive suicide prevention approach that prioritizes population impact. To realize the potential contribution of Wingman-Connect Program, additional longitudinal research is needed testing this program for impact on suicidal behaviors over longer follow-up periods. Work is also needed to identify effective practices for scalable implementation of the program.
Study concept and design: Wyman, Pickering, Cero, Acquisition, analysis or interpretation of data: Wyman, Pickering, Pisani, Cero, Yates, Schmeelk-Cone, Brown, Simonson, Pflanz, Drafting of the manuscript: Wyman, Pickering, Pisani, Cero, Schmeelk-Cone, Statistical analysis: Pickering, Cero, Schmeelk-Cone, Brown, Administrative, technical or material support: Wyman, Pisani, Brown, Yates, Schmeelk-Cone, Simonson, Pflanz, Study supervision: Wyman.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.114737.
Anderson, L., Campbell-Sills, L., Ursano, R.J., et al., 2019. Prospective associations of perceived unit cohesion with post-deployment mental health outcomes. Depress. Anxiety 36.
Brown, C.H., Wyman, P.A., Brinales, J.M., Gibbons, R., 2007. The role of randomized trials in testing interventions for the prevention of youth suicide. Int. Rev. Psychiatr. 19 (6), 617–631.
Brown, C.H., Wyman, P.A., Brinales, J.M., Gibbons, R., 2007. The role of randomized trials in testing interventions for the prevention of youth suicide. Int. Rev. Psychiatr. 19 (6), 617–631.
Burrell, L.M., 2006. Moving military families: the impact of relocation on family wellbeing, employment, and commitment to the military. In: Castro, C.A., Adler, A.B., Britt, T.W. (Eds.), Military Life: the Psychology of Serving in Peace and Combat: the Military Family, vol. 3. Praeger Security International, Westport, CT, pp. 39–63.
Campbell-Sills, L., Flynn, P.J., Choi, K.W., et al., 2020. Unit cohesion during deployment and post-deployment mental health: is cohesion an individual- or unit level buffer for combat-exposed soldiers? Psychol. Med.
Christakis, N.A., 2019. Blueprint: the Evolutionary Origins of a Good Society. Little, Brown Spark.
Comtois, K.A., Kerbrat, A.H., DeCou, C.R., et al., 2019. Effect of augmenting standard care for military personnel with brief caring text messages for suicide prevention: a randomized clinical trial. JAMA Psychiatr. 76 (5), 474–483.
Csardi, G., Nepusz, T., 2006. The igraph software package for complex network research. Inter J. Complex Syst. 1695 (5), 1–9.
IOM, 2013. Returning Home from Iraq and Afghanistan: Assessment of Readjustment Needs of Veterans, Service Members, and Their Families. Washington, D.C.
Frank, K.A., Maroulis, S.J., Duong, M.Q., Kelcey, B.M., 2013. What would it take to change an inference? Using Rubin’s causal model to interpret the robustness of causal inferences. Educ. Eval. Pol. Anal. 35 (4), 437–460.
Gibbons, R.D., Kupfer, D., Frank, E., Moore, T., Beiser, D.G., Boudreaux, E., 2017. Development of a computerized adaptive suicide scale: CAT-SS. J. Clin. Psychiatr. 78 (9), 1376–1382.
Griffith, J., 2015. Cross (unit)-level effects of cohesion on relationships of suicide thoughts to combat exposure, postdeployment stressors, and postdeployment social support. Behav. Med. 41 (3), 98–106.
Hoge, C.W., 2019. Suicide reduction and research efforts in service members and veterans – sobering realities. JAMA Psychiatr. 76 (5), 464–466.
Hom, M.A., Stanley, I.H., Schneider, M.E., Joiner, T., 2017. A systematic review of helpseeking and mental health service utilization among military service members. Clin. Psychol. Rev. 53, 59–78.
Leahy, R.L., 2018. Cognitive Therapy Techniques: A Practitioner’s Guide, 2 ed. Guildford Press, New York, NY.
Lutz, J., Van Orden, K.A., Bruce, M.L., Conwell, Y., 2021. Social disconnection in late life suicide: an NIMH workshop on state of the research in identifying mechanisms, treatment targets, and interventions. Am. J. Geriatr. Psychiatr.
Martin, J.S., Novak, L.A., Perera, K., et al., 2019. Suicide typologies in the United States Air Force: a hierarchical cluster analysis. Suicide Life-Threatening Behav. 49 (6), 1707–1720.
Mead, E.L., Rimal, R.N., Ferrence, R., Cohen, J.E., 2014. Understanding the sources of normative influence on behavior: the example of tobacco. Soc. Sci. Med. 115, 139–143.
Mueller, A.S., Abrutyn, S., Pescosolido, B., Diefendorf, S., 2021. The social roots of suicide: theorizing how the external social world matters to suicide and suicide prevention. Front. Psychol. 12.
Pickering, T.A., Wyman, P.A., Schmeelk-Cone, K., et al., 2018. Diffusion of a peer-led suicide preventive intervention through school-based student peer and adult networks. Front. Psychiatr. 9, 598.
Pruitt, L.D., Smolenski, D.J., Tucker, J., et al., 2018. Department of Defense Suicide Event Report (DoDSER): Calendar Year 2017 Annual Report. Department of Defense. https://www.dspo.mil/Portals/113/Documents/2017 DoDSERAnnual-Report.pdf?ver=2019-07-19-110951 577.
Pruitt, L.D., Smolenski, D.J., Bush, N.E., et al., 2019. Suicide in the military: understanding rates and risk factors across the United States’ armed forces. Mil. Med. 184, 432–437.
R_Core_Team, R., 2020. A Language and Environment for Statistical Computing. Vienna, Austria.
Rose, G., 1985. Sick individuals and sick populations. Int. J. Epidemiol. 14 (1).
Rudd, M.D., Bryan, C.J., Wertenberger, E.G., et al., 2015. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow up. Am. J. Psychiatr. 172 (5), 441–449.
Rugo, K.F., Leifker, F.R., Drake-Brooks, M.M., Snell, M.B., Bryan, C.J., Bryan, A.O., 2020. Unit cohesion and social support as protective factors against suicide risk and depression among National Guard service members. J. Soc. Clin. Psychol. 39, 214–228.
Schaefer, D.R., Kornienko, O., Fox, A.M., 2011. Misery does not love company: network selection mechanisms and depression homophily. Am. Socio. Rev. 76 (5), 764–785.
Silva, C., Hagan, C.R., Rogers, M.L., et al., 2016. Evidence for the propositions of the interpersonal theory of suicide among a military sample. J. Clin. Psychol. 73 (6), 669–680.
Tsai, A.C., Lucas, M., Kawachi, I., 2015. Association between social integration and suicide among women in the United States. JAMA Psychiatr. 72 (10), 987–993.
Valente, T.W., 2010. Social Networks and Health: Models, Methods and Applications. Oxford University Press, New York.
Valente, T.W., Fujimoto, K., Chou, C.P., Sprijt-Metz, D., 2009. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J. Adolesc. Health 45 (2), 202–204.
Van Orden, K.A., Witte, T.K., Cukrowicz, K.C., Braithwaite, S.R., Selby, E.A., Joiner, T., 2010. The interpersonal theory of suicide. Psychol. Rev. 117 (2), 575–600.
Wasserman, S., Faust, K., 1994. Social Network Analysis: Methods and Applications. Cambridge University Press, US, New York, NY.
Whitlock, J., Wyman, P.A., Moore, S.R., 2014. Connectedness and suicide prevention in adolescents: pathways and implications. Suicide Life-Threatening Behav. 44, 246–272.
Wyman, P.A., 2014. Developmental approach to prevent adolescent suicides: research pathways to effective upstream preventive interventions. Am. J. Prev. Med. 47, S251–S256.
Wyman, P.A., Pickering, T.A., Pisani, A.R., et al., 2019. Peer-adult network structure and suicide attempts in 38 high schools: implications for network-informed suicide prevention. JCPP (J. Child Psychol. Psychiatry) 60 (10), 1065–1075.
Wyman, Peter, Pisani, Anthony, Brown, CH, et al., 2020. Effect of Wingman-Connect upstream suicide prevention for Air Force personnel in training: A cluster randomized controlled trial. JAMA Open Network 3 (10). https://doi.org/10.1001/jamanetworkopen.2020.22532. In this issue.